Artificial human skin paves the way to new skin cancer therapy
In a new study, researchers have managed to curb skin cancer. The study was conducted on artificial human skin.

By using artificial human skin, a research group from the University of Copenhagen have managed to block invasive growth in a skin cancer model.
The study has been published in Science Signaling and looks at what actually happens when a cell turns into a cancer cell.
“We have been studying one of the cells’ signalling pathways, the so-called TGF beta pathway. This pathway plays a critical role in the cell’s communication with its surroundings, and it controls e.g. cell growth and cell division. If these mechanisms are damaged, the cell may turn into a cancer cell and invade the surrounding tissue,” explains Professor and Team Lead Hans Wandall from the Department of Cellular and Molecular Medicine at the University of Copenhagen.
By using artificial human skin we are past the potentially problematic obstacle of whether results from tests on mice models can be transferred to human tissue.
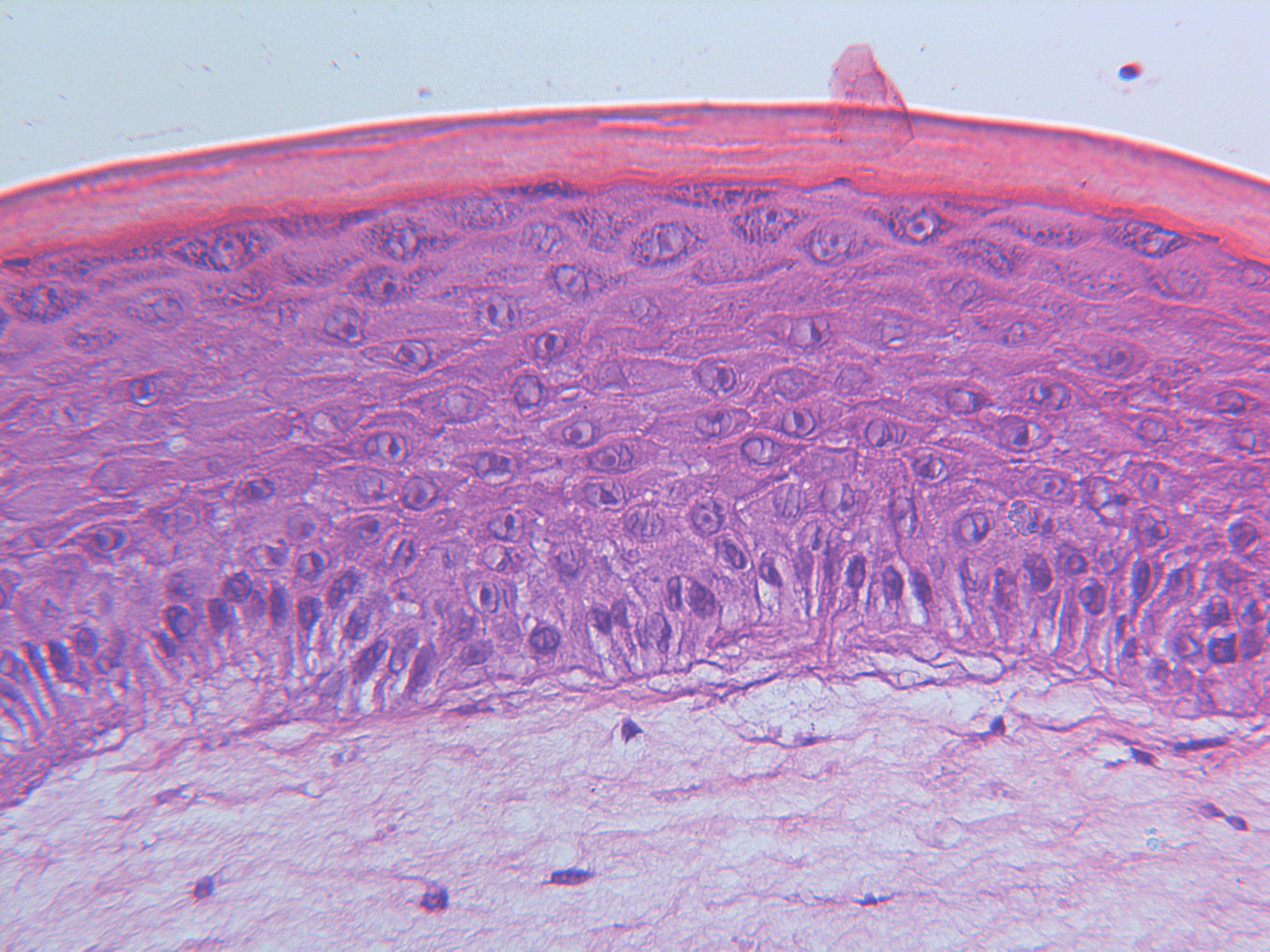
Under normal circumstances, your skin cells will not just start to invade the hypodermis and wreak havoc. Instead, they will produce a new layer of skin. But when cancer cells emerge, the cells no longer respect the boundaries between skin layers, and they start to invade each other. This is called invasive growth.
Hans Wandall and his colleagues have been studying the TGF beta pathway and applied methods for blocking invasive growth and thus curbing the invasive growth in skin cancer.
“We already have various drugs that can block these signalling pathways and which may be used in tests. We have used some of them in this study,” explains Associate Professor and co-author of the study Sally Dabelsteen from the School of Dentistry.
Hans Wandall and Sally Dabelsteen have worked together with Dr. Zilu Ye and Professor Jesper V. Olsen from the Novo Nordisk Foundation Center for Protein Research at the Faculty of Health and Medical Sciences.
“Some of these drugs have already been tested on humans, and some are in the process of being tested in connection with other types of cancer. They could also be tested on skin cancer specifically,” she says.
Artificial skin is the closest we get to real human skin
The artificial skin used by the researchers in the new study consists of artificial, genetically manipulated human skin cells. Skin cells are produced on subcutaneous tissue made of collagen. This makes the cells grow in layers, just like real human skin.
Unlike mice models, the skin model, which is another word for artificial skin, allows researchers to introduce artificial genetic changes relatively quickly, which provide insight into the systems that support skin development and renewal.
This way they are also able to reproduce and follow the development of other skin disorders, not just skin cancer.
“By using artificial human skin we are past the potentially problematic obstacle of whether results from tests on mice models can be transferred to human tissue. Previously, we used mice models in most studies of this kind. Instead, we can now conclude that these substances probably are not harmful and could work in practice, because the artificial skin means that we are closer to human reality,” says Hans Wandall.
The artificial skin used by the researchers resembles the skin used to test cosmetics in the EU, which banned animal testing in 2004. However, artificial skin does not allow the researchers to test the effect of a drug on the entire organism, Hans Wandall points out. Skin models like the one used here have been used by cosmetics companies since the mid-1980s.
“We can study the effect focussing on the individual organ – the skin – and then we reap experiences with regard to how molecules work, while we seek to determine whether they damage the structure of the skin and the healthy skin cells,” he says.
Read the full study here: ‘Characterization of TGF-β signaling in a human organotypic skin model reveals that loss of TGF-βRII induces invasive tissue growth’.
Contact
Associate Professor Sally Dabelsteen
+45 61 71 09 36
sdab@sund.ku.dk
